INR. 300
+918042754614
This is your website preview.
Currently it only shows your basic business info. Start adding relevant business details such as description, images and products or services to gain your customers attention by using Boost 360 android app / iOS App / web portal.
Description
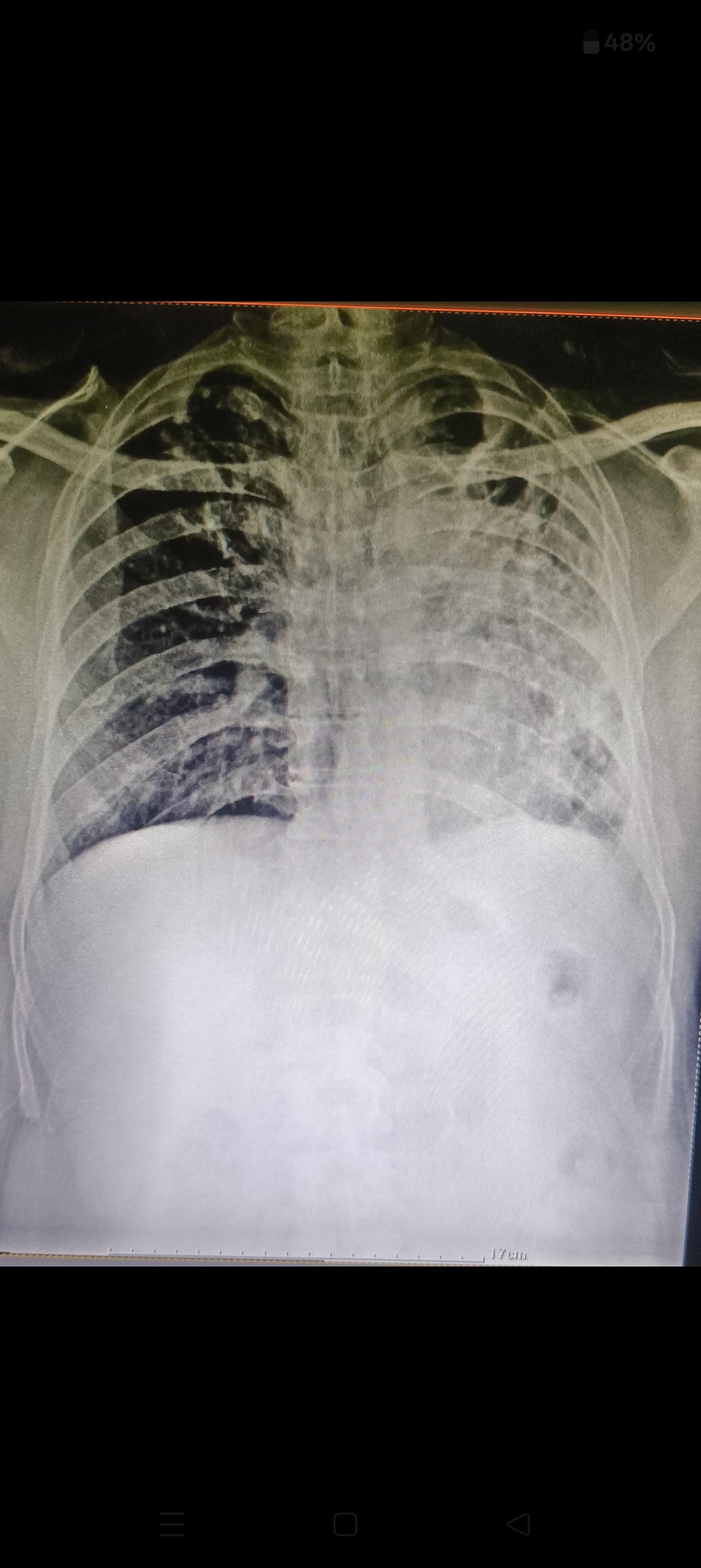
The term “Koch’s” refers to Pulmonary Tuberculosis (TB), named after Dr. Robert Koch, who discovered Mycobacterium tuberculosis. After TB infection is treated, some patients are left with residual structural damage in the lungs. --- 2. Pathology Fibrosis: Chronic TB inflammation heals by forming scar tissue. This scarring (fibrosis) makes the lung tissue stiff and nonfunctional. Collapse (Atelectasis): Fibrosis can pull on surrounding lung tissue and cause shrinkage (volume loss). Bronchial obstruction due to scarring can also contribute to collapse. Sequelae (after-effects of old TB): Cavities, bronchiectasis (damaged dilated bronchi), calcified nodes, and pleural thickening may be seen. Sometimes the entire lung may look “destroyed” on X-ray. --- 3. Clinical Features Patients with old healed TB sequelae may have: Chronic cough with scanty sputum. Breathlessness on exertion (due to reduced lung volume). Occasional hemoptysis (coughing blood, if bronchiectasis or damaged vessels). Chest asymmetry (sunken side if one lung collapsed). Often, many are asymptomatic and detected on routine chest X-ray. --- 4. Radiological Findings On Chest X-ray / CT Scan, typical features include: Fibrotic strands, volume loss. Mediastinal shift towards affected side. Rib crowding, elevation of diaphragm on that side. Calcification, pleural thickening. Bronchiectasis or cavities (if present). --- 5. Complications Secondary infections (due to poor lung clearance). Bronchiectasis → recurrent sputum production, hemoptysis. Pulmonary hypertension and cor pulmonale (right heart strain) in severe, bilateral cases. Rarely, reactivation TB in residual cavities. --- 6. Management Since fibrosis and collapse are irreversible, treatment focuses on: Rule out active TB → sputum AFB, GeneXpert, clinical correlation. Pulmonary rehabilitation → breathing exercises, physiotherapy. Vaccination (influenza, pneumococcal) to prevent infections. Bronchodilators & inhalers (if obstruction). Antibiotics for secondary infections. Hemoptysis management (antifibrinolytics, bronchial artery embolization if severe). Surgery (rare, only if localized destroyed lung with recurrent infection/hemoptysis).